Every audience I speak to brings a unique lens to blood flow restriction (BFR) training. At last month’s NFL meetings, the focus was on performance, recovery, and post-op protocols. At NASA, it was all about muscle and bone preservation in space. Last week, I presented at the NBA Combine in Chicago—where the spotlight shifts to high-frequency injuries in professional basketball: soft tissue strains, Achilles ruptures and, notably, ankle instability.
Chronic ankle instability (CAI) presents significant challenges for both patients and clinicians, affecting approximately 40% of individuals following an initial ankle sprain (Gribble et al., 2016). This condition is characterized by persistent symptoms including recurrent ankle sprains, episodes of "giving way," and functional deficits that can significantly impact athletic performance and daily activities. In professional basketball alone, ankle sprains account for over 25% of all injuries (Drakos et al., 2010), with CAI representing not just a nuisance but a genuine performance limiter.
Primary Deficits and Challenges
Strength Impairments
Patients with CAI typically exhibit reduced strength in the peroneal muscles, which are critical for lateral stability (Donovan & Hertel, 2012). This weakness often persists despite conventional rehabilitation protocols, creating a foundational deficit that contributes to ongoing instability. Traditional rehabilitation approaches frequently fail to adequately address deep muscle weakness and force production capabilities, particularly at functional speeds and in sport-specific movements (Kaminski et al., 2013).
Biomechanical Challenges in Traditional Strengthening
One of the fundamental biomechanical limitations in ankle rehabilitation relates to the short lever arm of the foot and ankle complex. Unlike larger proximal joints that can accommodate substantial external loading (such as the knee or hip), the distal nature and shorter lever length of the ankle make traditional progressive resistance training particularly challenging (Donovan & Feger, 2017). The mechanical disadvantage of this anatomical arrangement significantly limits the effective loads that can be safely applied, especially for critical lateral stabilizers like the peroneal muscles. Conventional strengthening often reaches a ceiling effect where further functional gains become difficult to achieve due to these loading limitations, creating a gap between rehabilitation exercise intensity and the demands of high-velocity, sport-specific movements (Kaminski et al., 2013). This biomechanical constraint represents a significant barrier to restoring complete functional strength and power in individuals with CAI, particularly when attempting to replicate the forces encountered during cutting, landing, and other dynamic sporting movements.
Balance and Proprioceptive Deficits
CAI is characterized by impaired proprioception and neuromuscular control, manifesting as poor balance and position awareness (Hertel, 2008). While balance training is commonly prescribed, conventional protocols often lack the specificity and progressive challenge needed to translate improvements to dynamic, sport-specific scenarios. Static balance improvements frequently fail to transfer to dynamic athletic movements, leaving athletes vulnerable during competition (McKeon & Hertel, 2008).
Return to Play Considerations
A significant limitation in current rehabilitation approaches is the lack of standardized, evidence-based criteria for return to play decisions (Clanton et al., 2012). Clinicians often rely on subjective assessments or basic functional tests that may not adequately reflect the demands of competitive sports. This gap between rehabilitation outcomes and sport demands contributes to premature returns and subsequent reinjuries (Wikstrom et al., 2013).
Reinjury Rates
Perhaps most concerning is the high rate of recurrence—up to 70% of athletes with CAI experience reinjury upon returning to sport (Anandacoomarasamy & Barnsley, 2005). This cycle of injury-rehabilitation-reinjury suggests fundamental limitations in current treatment protocols. Traditional rehabilitation often fails to address the complex interplay of mechanical instability, functional deficits, and psychological factors that contribute to reinjury risk (Hiller et al., 2011).
Limitations in Current Rehabilitation Approaches
Current rehabilitation protocols for CAI face several key limitations:
- Insufficient Loading Parameters: Traditional exercises often fail to provide adequate progressive overload to restore full strength and power in sport-specific movements (Lepley et al., 2018).
- Limited Neuromuscular Training Specificity: Many protocols emphasize basic balance exercises without progression to sport-specific neuromuscular challenges that replicate competitive demands (McKeon et al., 2014).
- Inadequate Addressing of Mechanical Instability: Rehabilitation frequently focuses on functional components while undertreating the structural contributors to instability (Delahunt et al., 2010).
- Psychological Readiness Overlooked: Fear of reinjury and lack of confidence are rarely systematically addressed, despite their significant impact on movement patterns and reinjury risk (Houston et al., 2014).
- Poor Integration of Sensorimotor Training: Rehabilitation often separates strength and proprioceptive training rather than integrating them to develop functional stability during complex movements (Needle et al., 2017).
- Limited Long-term Approaches: Most protocols focus on short-term symptom resolution rather than long-term prevention strategies, contributing to the high recurrence rates (Donovan & Hertel, 2012).
Blood Flow Restriction Training: A Novel Intervention for CAI
Emerging research suggests that Blood Flow Restriction (BFR) training represents a promising novel intervention that directly addresses many of the limitations in conventional CAI rehabilitation. What began as a theoretical application has evolved into an evidence-supported tool with substantial potential for ankle rehabilitation.
Several years ago, we hypothesized that BFR could be particularly beneficial for chronic ankle instability, but at that time there were no published papers specifically examining this application (Faltus et al., 2018). What began as a theoretical model has evolved into an evidence-supported tool with substantial potential for ankle rehabilitation.

BFR training offers unique advantages in addressing the complex deficits associated with CAI. As we outlined in our previous work, BFR can help overcome the biomechanical challenge of the ankle's short lever arm by enabling greater strength and hypertrophy adaptations at lower mechanical loads (typically 20-30% of maximum), effectively circumventing the "ceiling effect" that conventional strengthening encounters due to the ankle's mechanical disadvantage (Faltus et al., 2018). This approach creates what we've recently described as a mismatch between "external load" (the physical work performed during exercise) and "internal load" (the physiological and perceptual responses to exercise), allowing clinicians to elicit high internal training responses despite using low external loads that respect the biomechanical constraints of the ankle (Bielitzki et al., 2024).
Emerging Evidence Base
Seven published studies involving 184 CAI subjects demonstrate that BFR training can lead to significant improvements in lower-leg strength, balance, neuromuscular activation, range of motion, and self-reported function. These findings suggest BFR may offer a systematic approach to addressing the complex deficits associated with CAI.
Key research findings highlight BFR's multifaceted benefits:
- Enhanced Neuromuscular Activation: Killinger et al. (2019) demonstrated significant increases in EMG activation during ankle eversion and dorsiflexion exercises with BFR, suggesting improved motor unit recruitment—a critical factor in restoring dynamic stability.
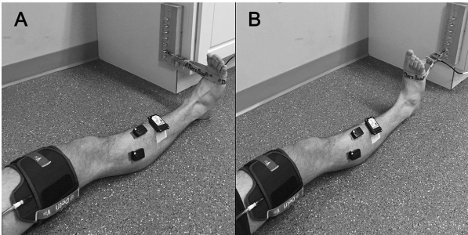
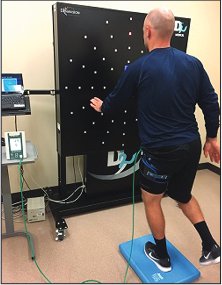
Killinger et al 2019
- Superior Strength Development: Nagdi et al. (2024) found 67-73% strength gains in dorsiflexors and plantarflexors with BFR combined with proprioceptive training, compared to more modest improvements with proprioception alone. Patient-reported outcomes (FAAM scores) improved 24% with BFR versus 13% in controls.
- Intensified Neuromuscular Challenge: Burkhardt et al. (2021) revealed that BFR during balance activities creates an "internal perturbation," enhancing muscle activation in the vastus lateralis and soleus while increasing perceived exertion and instability—effectively challenging the sensorimotor system in ways standard training cannot achieve.
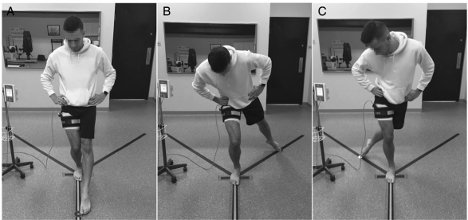
Burkhardt et al 2021
- Fatigue Resistance Training: Clark et al. (2024) demonstrated that BFR during the Star Excursion Balance Test simulates late-game fatigue, potentially training sensorimotor adaptability under challenging conditions that better reflect competitive demands.
- Comprehensive Functional Improvements: Multiple studies (Werasirirat & Yimlamai, 2022; Kim et al., 2023; Liu & Wang, 2024) have shown that integrating BFR with traditional rehabilitation elements produces superior outcomes in strength, hypertrophy, dynamic balance, range of motion, and patient-reported function.
Addressing Rehabilitation Gaps
BFR appears to address several critical limitations in traditional CAI rehabilitation:
- Optimized Loading: BFR enables greater strength and hypertrophy adaptations at lower mechanical loads (typically 20-30% of maximum), directly addressing the biomechanical limitation of the ankle's short lever arm that restricts effective loading in traditional rehabilitation. By creating metabolic stress and cellular swelling with reduced mechanical load, BFR circumvents the "ceiling effect" that conventional strengthening encounters due to the ankle's mechanical disadvantage, allowing for continued strength development without the need for potentially harmful high external loads (Patterson et al., 2019).
- Enhanced Neuromuscular Training: BFR creates a unique neurophysiological challenge that naturally integrates strength and proprioceptive training through what we recently published as a mismatch between "external load" and "internal load" (Bielitzki et al., 2024). In traditional ankle rehabilitation, static balance exercises represent a relatively low external load (the physical work performed during exercise), but when combined with BFR, they generate significantly higher internal load (the physiological and perceptual responses to exercise). Our research has shown that BFR during balance activities creates an "internal perturbation" that substantially increases muscle activation in the vastus lateralis and soleus while simultaneously increasing perceived exertion and instability (Burkhardt et al., 2021). This neurophysiological challenge cannot be achieved with standard training, as applying BFR effectively transforms low external load balance exercises into high internal load neuromuscular training. This approach is particularly valuable for ankle rehabilitation, given the biomechanical limitation of the ankle's short lever arm, which restricts the application of progressive external loads. By focusing on manipulating internal load through BFR rather than increasing mechanically limited external loads, clinicians can more effectively challenge the sensorimotor system while maintaining safe mechanical stress on healing tissues.
- Integrated Sensorimotor Challenge: BFR naturally combines strength and proprioceptive training by creating what neuroscientists call "afferent-efferent coupling." During BFR balance activities, the metabolite accumulation stimulates type III and IV afferent fibers, which simultaneously increases the central nervous system's activation of motor pathways (Burkhardt et al., 2021). This neurophysiological mechanism creates a dual challenge: the muscles must work harder (increased efferent output) while the brain receives altered sensory information (modified afferent input).
In simpler terms, BFR balance exercises require the brain to maintain stability while receiving unusually challenging sensory signals and commanding muscles that are experiencing accelerated fatigue. This is particularly valuable because traditional balance training often separates strength from proprioception, while BFR seamlessly integrates them in a single exercise. The proprioceptive system learns to maintain stability despite growing muscle fatigue – precisely the challenge athletes face in late-game situations when ankle injuries commonly occur.
This integrated sensorimotor approach addresses a fundamental limitation in traditional CAI rehabilitation, where exercises typically target either strength OR balance in isolation. Research shows that BFR during simple balance tasks produces similar neuromuscular recruitment patterns to those seen during complex, high-load functional movements (Bielitzki et al., 2023), allowing clinicians to train functional stability with less mechanical stress on healing tissues. The end result is a more efficient neuromuscular system that can maintain ankle stability even as muscles fatigue throughout athletic competition. - Functional Performance Transfer: The improvements in patient-reported outcomes suggest that BFR-induced adaptations translate effectively to real-world functional performance, bridging the critical gap between clinical measures and meaningful patient experience.
When examining the research, we see that patients with CAI who undergo BFR training report significantly greater improvements in self-perceived function compared to those in conventional training groups. For example, Nagdi et al. (2024) documented a 24% improvement in Foot and Ankle Ability Measure (FAAM) scores with BFR versus only 13% with standard proprioceptive training. These results are particularly meaningful because they reflect the patient's own assessment of how their ankle functions during daily activities and sport-specific movements.
From a clinical perspective, these enhanced patient-reported outcomes provide several significant advantages. First, they serve as a powerful motivational tool, as patients who perceive tangible improvements in function tend to demonstrate greater adherence to rehabilitation programs. When patients can feel the difference in their ankle stability during basketball-specific movements like cutting, pivoting, and landing, they're more likely to maintain their therapeutic exercise regimen.
Second, improved self-reported function correlates strongly with psychological readiness to return to sport—a critical but often overlooked component of successful rehabilitation. Athletes with CAI frequently develop fear-avoidance behaviors and decreased confidence in their ankle, which can persist even after objective measures have normalized. The robust improvements in patient-perceived function with BFR training may help restore this confidence more effectively than traditional approaches.
Third, these outcomes allow clinicians to better monitor rehabilitation progress from the patient's perspective. By tracking tools like the FAAM, Cumberland Ankle Instability Tool (CAIT), or Identification of Functional Ankle Instability (IdFAI), therapists can quantify subjective improvements and adjust treatment plans accordingly. This patient-centered approach ensures that rehabilitation addresses the functional limitations that matter most to the individual athlete, rather than focusing solely on clinical measures that may not translate to performance.
For basketball players specifically, the transfer to functional performance often means they can return to sport with greater confidence in their ankle's stability during high-demand movements like defensive slides, rebounding, and jump landings. This functional confidence is invaluable in preventing the hesitancy and altered movement patterns that often lead to reinjury or compensatory injuries elsewhere in the kinetic chain.
By generating improvements that patients can feel and measure in their daily lives and sport performance, BFR training helps close the often-frustrating gap between clinical recovery and functional return to sport that has traditionally challenged CAI rehabilitation.
Conclusion
While research on long-term outcomes and re-injury rates is still developing, the current evidence base strongly suggests that BFR represents a valuable, evidence-informed tool that can be strategically integrated into comprehensive CAI rehabilitation protocols. For clinicians seeking to overcome the limitations of traditional approaches, BFR offers a systematic method to enhance strength, balance, and functional outcomes for individuals struggling with chronic ankle instability.
By Johnny Owens, MPT
References
Anandacoomarasamy, A., & Barnsley, L. (2005). Long term outcomes of inversion ankle injuries. British Journal of Sports Medicine, 39(3), e14.
Bielitzki, R., Behrens, M., Behrendt, T., Franz, A., Centner, C., Hughes, L., Patterson, S. D., Owens, J., Behringer, M., & Schega, L. (2024). The discrepancy between external and internal load/intensity during blood flow restriction exercise: Understanding blood flow restriction pressure as modulating factor. Sports Medicine - Open, 10(95), 1-11.
Burkhardt, E., Akins, J., Valenzuela, K., McGrath, M., & Johnson, S. (2021). Effects of blood flow restriction on dynamic balance: A crossover study. Journal of Sport Rehabilitation, 30(5), 735-742.
Clark, B.C., Ford, K.R., Uhl, T.L., & Johnson, B.T. (2024). Blood flow restriction during the Star Excursion Balance Test affects performance and perceived stability. Physical Therapy in Sport.
Clanton, T. O., Matheny, L. M., Jarvis, H. C., & Jeronimus, A. B. (2012). Return to play in athletes following ankle injuries. Sports Health, 4(6), 471-474.
Delahunt, E., Coughlan, G. F., Caulfield, B., Nightingale, E. J., Lin, C. W., & Hiller, C. E. (2010). Inclusion criteria when investigating insufficiencies in chronic ankle instability. Medicine and Science in Sports and Exercise, 42(11), 2106-2121.
Donovan, L., & Feger, M. A. (2017). Relationship between ankle frontal plane kinematics during different functional tasks. Gait & Posture, 54, 214-220. doi: 10.1016/j.gaitpost.2017.03.017
Donovan, L., & Hertel, J. (2012). A new paradigm for rehabilitation of patients with chronic ankle instability. Physician and Sportsmedicine, 40(4), 41-51.
Drakos, M. C., Domb, B., Starkey, C., Callahan, L., & Allen, A. A. (2010). Injury in the National Basketball Association: a 17-year overview. Sports Health, 2(4), 284-290.
Faltus, J., Owens, J., & Hedt, C. (2018). Theoretical applications of blood flow restriction training in managing chronic ankle instability in the basketball athlete. International Journal of Sports Physical Therapy, 13(3), 552-560. doi: 10.26603/ijspt20180552
Gribble, P. A., Bleakley, C. M., Caulfield, B. M., Docherty, C. L., Fourchet, F., Fong, D. T., ... & Delahunt, E. (2016). Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. British Journal of Sports Medicine, 50(24), 1496-1505.
Hertel, J. (2008). Sensorimotor deficits with ankle sprains and chronic ankle instability. Clinics in Sports Medicine, 27(3), 353-370.
Hiller, C. E., Kilbreath, S. L., & Refshauge, K. M. (2011). Chronic ankle instability: evolution of the model. Journal of Athletic Training, 46(2), 133-141.
Houston, M. N., Van Lunen, B. L., & Hoch, M. C. (2014). Health-related quality of life in individuals with chronic ankle instability. Journal of Athletic Training, 49(6), 758-763.
Hughes, L., Paton, B., Rosenblatt, B., Gissane, C., & Patterson, S. D. (2017). Blood flow restriction training in clinical musculoskeletal rehabilitation: a systematic review and meta-analysis. British Journal of Sports Medicine, 51(13), 1003-1011.
Kaminski, T. W., Hertel, J., Amendola, N., Docherty, C. L., Dolan, M. G., Hopkins, J. T., ... & Richie, D. (2013). National Athletic Trainers' Association position statement: conservative management and prevention of ankle sprains in athletes. Journal of Athletic Training, 48(4), 528-545.
Killinger, B., Lauver, J. D., Calvert, L., & Donovan, L. (2019). Blood flow restriction increases muscle activation during submaximal exercise in individuals with chronic ankle instability. Journal of Electromyography and Kinesiology, 45, 11-17.
Kim, S. J., Cho, J. H., & Kim, S. H. (2023). Effects of blood flow restriction training combined with active joint mobilization on dynamic balance and muscle activation in patients with chronic ankle instability. Journal of Back and Musculoskeletal Rehabilitation, 36(1), 187-196.
Lepley, L. K., Davi, S. M., Burland, J. P., & Lepley, A. S. (2018). Importance of muscle strength in the management of chronic ankle instability. Foot & Ankle Specialist, 11(2), 175-181.
Liu, C., & Wang, X. (2024). Effects of blood flow restriction combined with instrument-assisted soft tissue mobilization and exercise on chronic ankle instability: A randomized controlled trial. Journal of Sport Rehabilitation.
McKeon, P. O., & Hertel, J. (2008). Systematic review of postural control and lateral ankle instability, part II: is balance training clinically effective? Journal of Athletic Training, 43(3), 305-315.
McKeon, P. O., Ingersoll, C. D., Kerrigan, D. C., Saliba, E., Bennett, B. C., & Hertel, J. (2014). Balance training improves function and postural control in those with chronic ankle instability. Medicine & Science in Sports & Exercise, 46(8), 1559-1567.
Nagdi, S. A., Gad, A. M., & Saleh, A. K. (2024). Effect of blood flow restriction on ankle proprioception in athletes with chronic ankle instability. Journal of Bodywork and Movement Therapies, 37, 101-109.
Needle, A. R., Kaminski, T. W., Baumeister, J., Higginson, J. S., Farquhar, W. B., & Swanik, C. B. (2017). The relationship between joint stiffness and muscle activity in unstable ankles and copers. Journal of Sport Rehabilitation, 26(1), 15-25.
Patterson, S. D., Hughes, L., Warmington, S., Burr, J., Scott, B. R., & Owens, J. (2019). Blood flow restriction exercise: Considerations of methodology, application, and safety. Frontiers in Physiology, 10, 533.
Werasirirat, P., & Yimlamai, T. (2022). Effects of blood flow restriction training on muscle strength, hypertrophy, and functional performance in patients with chronic ankle instability. Physical Therapy in Sport, 56, 204-211.
Wikstrom, E. A., Hubbard-Turner, T., & McKeon, P. O. (2013). Understanding and treating lateral ankle sprains and their consequences. Sports Medicine, 43(6), 385-393.


