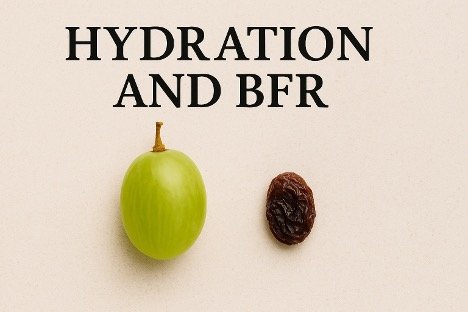
After years of implementing blood flow restriction training in clinical settings, I can confidently say that BFR is remarkably safe when performed correctly, with minimal reported adverse events. However, two incidents in my experience, along with similar reports from our clinical community, have changed how I think we should approach pre-session screening—and they all involve the same overlooked factor.
My Wake-Up Call
The first case involved an individual who became severely lightheaded and nearly unresponsive during what should have been a routine BFR session. She didn't lose consciousness, but the episode was concerning enough to immediately stop the session. When I questioned her afterward, she mentioned she'd recently been sick. She was worked up at her medical facility shortly after the incident and her urine specific gravity revealed that she was significantly dehydrated.
The second incident occurred with a patient who had an almost identical presentation: sudden onset lightheadedness during BFR, becoming nearly unresponsive but not fully syncopal. Again, post-episode questioning revealed recent illness (flu) and poor fluid intake over the preceding days.
Both individuals had completed their usual subjective screening without red flags. Both reported normal perceived exertion and pain levels right up until the vasovagal response occurred. The only common thread was dehydration following recent illness. As mentioned above, we have also had reports, very few but enough that we should take notice, from other clinicians performing BFR.
Our traditional monitoring methods might be missing a critical piece of the safety puzzle.
A recent study has helped confirm my experience (indirectly)
A recent June 2025 publication from our friend Dr. Jamie Burr's research team, led by McCrone et al.¹, examined how mild dehydration (~2% body mass loss) affects BFR exercise tolerance.
The Expected Finding: Dehydration didn't significantly change how hard the exercise felt or how much pain participants experienced during BFR walking.
The Possibly More Important Finding: However, four participants experienced pre-syncopal symptoms (lightheadedness, nausea) during the dehydrated trial—all of whom completed the identical protocol without incident when properly hydrated.
This confirms what I learned the hard way: perceived effort and pain aren't reliable predictors of hemodynamic stress when hydration is compromised. Patients might feel "fine" right up until they experience a vasovagal episode.
The Perfect Storm for Vasovagal Events
Here's why dehydration creates the ideal conditions for problems during BFR:
- Reduced plasma volume from fluid loss
- Venous pooling from cuff inflation
- Compromised cerebral perfusion when these factors combine
- Autonomic nervous systems inability to maintain blood pressure
Even modest dehydration can trigger this cascade in susceptible individuals—and there's really no way to predict who's at risk based on how they feel during exercise.
Clinical Reality Check
In their recent BFR Guidelines, the Australian Institute of Sport explicitly recommends against performing BFR in a dehydrated state, citing increased cardiovascular and thrombotic risks². It’s not about extreme dehydration—even mild fluid deficits can create problems.
Key Insight: Traditional monitoring (RPE, pain scales) may give you false confidence. A patient reporting low discomfort could still be at risk for sudden cardiovascular compromise if they're dehydrated.
Simple Hydration Screening Protocol
From this, I feel hydration assessment should become part of our pre-BFR checklist for every single session:
At a Minimum do a Quick Subjective Screen:
- "Have you had a couple glasses of water in the last 2-3 hours?"
- "Is your urine clear or light yellow?"
- "Do you feel thirsty, lightheaded, or dry-mouthed?"
- "Have you been sick recently or had any illness in the past week?"
Objective Checks When Possible:
- Urine charts: Dark yellow = likely dehydrated
- Body weight: Down >1% from baseline = concerning
- Urine specific gravity: >1.020 suggests dehydration
High-Risk Situations (Extra Vigilance Required):
- Recent illness or recovery from flu/cold
- Early morning sessions
- Post-travel
- Hot environments
- Recent alcohol consumption
- Older adults or post-operative patients
The Bottom Line
BFR is a very safe intervention, but these experiences taught me that hydration screening should be as routine as checking cuff placement or determining limb occlusion pressure. This recent research confirms what I learned through clinical experience: hydration status may not change how BFR feels, but it absolutely influences how the body tolerates the intervention.
Don't let this hidden risk factor compromise your BFR outcomes—or put your patients at unnecessary risk.
References:
- McCrone JC, Pignanelli C, Lydiate GC, et al. The effects of body hydration on perceptual responses during blood flow restriction exercise. Physiological Reports. 2025;13:e70343. https://doi.org/10.14814/phy2.70343
- Australian Institute of Sport. Blood Flow Restriction Training Guidelines. Australian Sports Commission; 2019. Available at: https://www.ais.gov.au/position_statement/blood_flow_restriction_training